Order from us for quality, customized work in due time of your choice.
Community Chronic Ailments Concern
In the last five years, the morbidity rates for cancer and other chronic ailments have been on the rise within the Lauderdale Lakes Community. For instance, the incidence rate for cancer has risen from 22 per 1000 per year in 2004 to 28 per 1000 per year in 2015. The mortality rate for cancer has increased from 32 per 100,000 to 48 per 100,000 from 2004 to 2015. As indicated in the government data, only 49.9 percent of the population is enlisted in the affordable cancer-preventive health care services. In this research, the population of interest is the African American community.
The African American population is spread evenly within the Lauderdale Lakes Community. Specifically, the African American community occupies the Connecticut and Blue Hills neighborhoods. The population density of the City of Lauderdale is 8,831 per square mile. The average house unit density is 6,180 per square mile. There are about 9,000 households occupied by African Americans within this city. The average size of each household is 2.8. Due to the poverty level of 20%, the average income per household is $3,000 per month. The household income is $32,135 per year while the median income per family is $36,188. The per capita income is $16,775 on average within this family. In terms of the level of education, the community literacy level is at 80%. The employment rate stands at 69 percent. Those in the informal sector account for 49 percent while those in the private sector account for 51% of the population.
How it affects society
Even though health facilities within the Lauderdale Lakes Community have implemented numerous interventions to manage cancer prevalence, little effort has been carried out in terms of implementation. The current intervention mechanism has loopholes that implementers may take advantage of (Allan, Ball, & Alston, 2007). For instance, moral and financial support services are limited to pre-treatment care. This means that a large population is exposed to health and psychological complications associated with cancer. Since the majority of the African American population are relatively poor, they cannot afford constant health checkups and would only prefer the treatment-based healthcare alternative when sick.
The majority of the population has not embraced preventive health care practices, characterized by visiting the hospitals for checkups even when not feeling sick. As a result of the treatment culture in seeking healthcare services, cases of cancer are detected at advanced stages and little can be done to help this group (Allan, Ball, & Alston, 2007). Poor income is a serious impediment towards treating cancer and other chronic ailments. Specifically, the average income is at $3,000 per month is very low. As a result, healthy living through proper dieting and canceling is largely above the reach of this group. The incidence rate for cancer has risen from 22 per 1000 per year in 2004 to 28 per 1000 per year in 2015. This explains the rising trend in new cases of cancer reported within this population.
Recommendation
Intervention approach
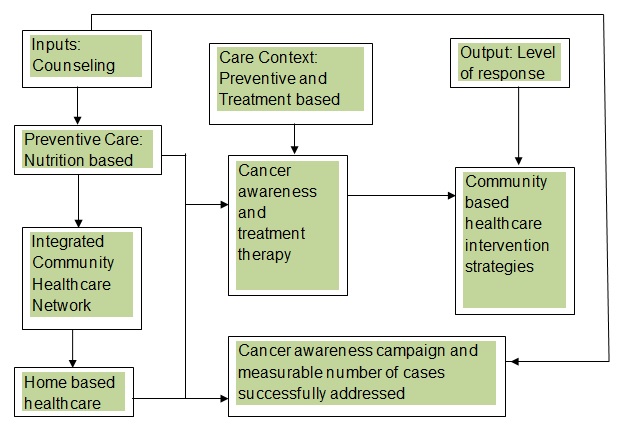
The intervention strategy will dwell on three main building blocks, which are preventive care, home-based care, and treatment-based care. Through these elements, the community health partners will have an opportunity to implement the triangular intervention mechanism. The output of the intervention will be measured by the level of positive response and the number of homes covered (Allan, Ball, & Alston, 2007). The elements of counseling home-based care and integrated community-based support play a key role in successful cancer intervention as summarized in the table below.
The Community Resources and Partners
The notable partners in the fight against cancer within the Lauderhill neighborhood are the Relay for Life, Caregiver, and Lung Cancer Alliance organization. These organizations promote preventive cancer care rather than the treatment option at an advanced stage. Besides, the government of the United States has enrolled a policy on chronic ailments to help curb the rising cases of cancer within this community.
Proposed government interventions
Simplifying administrative systems is vital towards reducing the high cost of cancer healthcare provision (Fielding & Briss, 2006). There is an urgent need to improve the extended Medicare safety to facilitate the management of Medicare for cancer patients and their families, who are equally affected (Allan, Ball, & Alston, 2007). Through subsidies on items that attract big fees to the cancer drug users, the medical providers in the Lauderdale Lakes Community will ultimately reduce consultation and medical fee. Streamlining the Lauderdale Lakes Community cancer clinics program would facilitate removal of uncommitted funding, which is important in operational activities (Allan, Ball, & Alston, 2007). When the activities are carried out through Medicare Network, a lot of savings will go to other supportive care activities for the cancer patients and their families. The local federal agency should opt for ‘active purchasing’ to leverage a secure bargaining power for the most competitive premium rates for the expensive cancer drugs. This will make the drugs affordable to those fighting cancer within the Lauderdale Lakes Community (Fielding & Briss, 2006).
Performance indicators in home-based cancer care are a means of fast-tracking goal achievement, understanding the position of the cancer policy in performance ladder, and allocating percentages as desired by the initiatives put in place. In the cancer healthcare management, the need for cost-effective healthcare management will ensure that preventive cancer education is integrated in the current community’s health programs (Casey & Wallis, 2011).
Proposed nursing actions
Through the ecological community-based approach in the cancer ailment prevention and treatment strategy, the goal would be to reduce the number of deaths caused by cancer (Casey & Wallis, 2011). The objectives of this approach are sensitization of cancer towards preventive care, provision of free checkup on a quarterly basis, and fast-tracking of the results of treatment through a voluntary follow-up for treating patients. Adoption of such objectives will leverage the health benefits to spread all costs of health recovery for the community (Allan, Ball, & Alston, 2007). As a result, the cost per individual will substantially decrease by a big margin.
As the nursing fraternity, it would be necessary to roll out community-based initiatives for addressing the normative and comparative needs of those infected and affected by the cancer menace. Normative needs represent the standard state of variances between a group and individuals sharing the same average summation criterion (Casey & Wallis, 2011). On the other hand, a comparative need is the quantifiable discrepancy that may exist in group as compared to others that share characteristics that are similar. Therefore, normative need in this case would be the standard of treatment for the individual asset in the service charter for addressing cancer and other chronic ailments in the community (Chisholm & Evans, 2007). Comparative need here would be spreading the intervention strategies uniformly across the subjects. The objective of this approach is sensitization of cancer towards preventive care; provision of free check up on a quarterly basis and fast-tracking the results of treatment through a voluntary follow-up for treating patients (Lewis, 2011).
Outcome evaluation
Evaluation of the outcome will encompass process evaluation, impact evaluation, and outcome evaluation of the preventive health care strategy for addressing cancer concern within the Lauderdale Lakes Community. Process evaluation will examine actual implementation and development within a specific program. In this case, success of evaluation will depend on response rate to the strategies adopted to address the chronic ailments concern within the Lauderdale Lakes Community. Specifically, the success will rely on the number of persons embracing the preventive community-based health care strategy (Olson et al., 2009). Reflectively, it will review quantifiable fulfillment of targets of the program. Though done at the end of this program, it will evaluate all aspects from commencement to completion. On the other hand, impact evaluation will examine long-term changes that have surfaced as part of the success or failure of a project (Allan, Ball, & Alston, 2007). It examines the long-term effectiveness of policy based programs after implementation. Outcome evaluation will examine the degree of change that has been witnessed due to successful implementation of the proposed cancer intervention program.
References
Allan, J., Ball, P., & Alston, M. (2007). Developing sustainable models of rural health care: A community development approach. Rural and Remote Health, 7(3), 818- 819.
Casey, A., & Wallis, A. (2011). Effective communication: principle of nursing practice. Nursing Standard, 25(32), 35-37.
Chisholm, D., & Evans, D. (2007). Economic evaluation in health: saving money or improving care? Journal of Medical Economics, 10(8), 325-337.
Fielding, J. & Briss, P. (2006).Promoting evidence-based public health policy: Can we have better evidence and more action? Health affairs, 25(4), 969-978.
Lewis, L. M. (2011). Medication adherence and spiritual perspectives among African American older women with hypertension. Journal of Gerontological Nursing, 37(6), 34-41.
Olson K., Susan, S., Betty, L., & Marjorie, S. (2009). Population-based public health interventions: Practice-based and evidence supported. Public Health Nursing, 21(5), 453-468.
Order from us for quality, customized work in due time of your choice.