Order from us for quality, customized work in due time of your choice.
Assessment
In order to ensure that a nurse possesses the ability to perform certain health care related tasks in the clinical setting, it is necessary to conduct an assessment of clinical competencies on a regular basis. Therefore, health care organizations aiming at the achievement of superior patient care outcomes continuously monitor and regularly assess clinical competencies of their staff. An assessment of clinical competencies could be performed by clinical nurse specialists, nurse managers or nurse educators (Schub & Heering, 2016). However, it is the responsibility of nursing managers to keep the records of regular clinical competency assessments. The desired outcome of an assessment of clinical competencies is to “gain a realistic view of whether a nurse has the necessary skills and knowledge to consistently perform clinical tasks that are within his or her expected scope of practice” (Schub & Heering, 2016, p. 103).
The aim of this paper is to develop an assessment plan on the basis of the Objective Structured Clinical Examination (OSCE) model. It will critique the design of OSCE model and will adjust it for the neurological assessment in order to make sure that it allows to adequately evaluate “a nurse’s ability to perform a task based on clinical skills, knowledge, education, and experience” (Schub & Heering, 2016, p. 103). The paper will provide a detailed analysis of the assessment progression. It will also present the methods for ensuring the validity, reliability, and practicality of the chosen assessment instruments.
OSCE
The OSCE model was developed in 1975 by Harden (Mcwilliam & Botwinski, 2012). It is an evaluation of performance that allows observing students in a simulated environment as they demonstrate a wide range of clinical behaviors. The OSCE model requires the participation of standardized patients (SPs) that have been trained to play a role of a person with a medical condition. SPs allow nursing students to show their knowledge and skills in an accurate and interactive training environment in order to demonstrate “assessment and the planning, implementation, and evaluation of care given in response to a single patient encounter” (Mcwilliam & Botwinski, 2012, p. 37).
The OSCE model is associated with the ability to recreate simulated experiences for multiple assessments thereby ensuring their objectivity. However, unlike the Structured Observation and Assessment of Practice (SOAP) model, it lacks a real clinical context. Taking into consideration the fact that assessment of clinical competencies has to include “contextualized, complex challenges, not fragmented tasks” (as cited in Levett-Jones, Gersbach, Arthur, & Roche, 2011, p. 66) it could be argued that the OSCE model lacks authenticity. However, due to the limited resources in the majority of clinical or educational settings, SOAP model is not the most practical tool for assessment. Therefore, the OSCE model has been chosen; however, in order to effectively use this method for neurological assessment, it has to be modified.
It should be mentioned that various accrediting agencies are concerned with the exploration of different methods for evaluating the performance of nursing graduates in order to make sure that students are prepared to engage in safe interaction with patients or clients. Specialized governmental bodies such as the Commission on Accreditation of Physical Therapy Education (CAPTE) are concerned with developing accreditation standards that help to ensure that educational organizations have systems that help to provide their students with sequential learning opportunities in accordance with standardized student outcomes (Gorman & Lazaro, 2011). For example, F-21 is one of the criteria developed by CAPTE, and it is directly related to the theme of this assignment. F-21 is associated with the evaluation of “student readiness to engage in clinical education” (Gorman & Lazaro, 2011, p. 63).
Therefore, an OSCE is usually placed at the end of a particular part of a program or curriculum in order to make sure that students have the skills necessary for safe interaction with patients. Under the OSCE model, professional actors or real patients are used for performing the role of SPs (Gorman & Lazaro, 2011). However, it could be argued that hired actors usually receive the amount of training that is not sufficient for an adequate understanding of case scenarios. Therefore, in order to conduct a proper neurological assessment, it is necessary to modify the OSCE model by employing registered nurses (RNs) as SPs. It will help to make sure that the role of patients is portrayed by people who have the experience necessary to deliver case scenarios without weakening OSCE format. Moreover, the standard OSCE model could be modified to include practice sessions with nurses playing the role of SPs where their performance would be assessed by a facilitator who could help them to better portray a patient without providing unintended feedback to students that could interfere with the process of their evaluation.
Development
The primary goal of the proposed OSCE assessment method is to make sure that students are ready to perform various tasks related to clinical patient management and including direct intervention and instruction (Selim, Ramadan, El-Gueneidy, & Gaafer, 2012). The process of the OSCE planning starts with the development of specific content areas that will be used for the creation of patient examination stations. The patient examination stations will help to determine students’ ability to perform clinical tasks covered by relevant content areas. In order to evaluate the OSCE, scoring checklists for each scenario will be developed. In addition to the use of SPs, written methods of examination will be used. It will help to make sure that more varied approach to the assessment is taken. An examination blueprint will include eight stations: patient interaction and written scenarios. The following patient stations utilizing standard patient interactions will be used: cranial nerve, motor system, cerebellum, deep tendon reflexes, sensation, and mental status examination (Estes, 2013). The remaining stations will include written scenarios containing questions pertaining to different aspects of interpreting documents, charts, and reports.
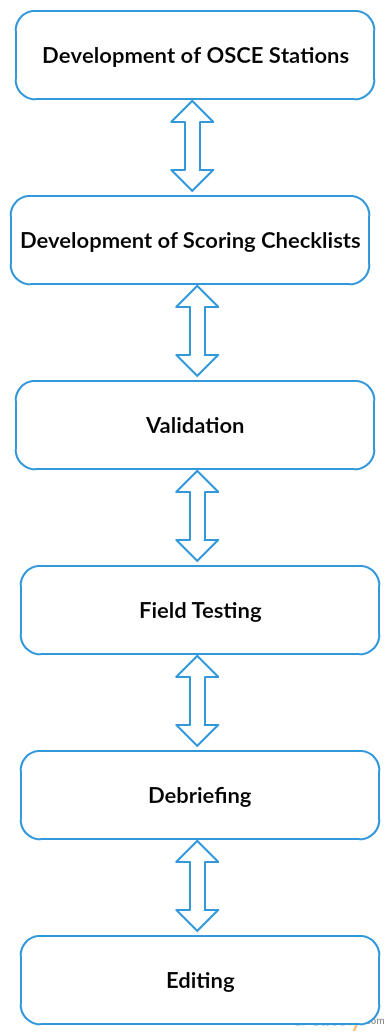
In order to ensure the validity, reliability, and practicability of the OSCE stations, the content of both written and standard patient interactions scenarios will be checked by a panel of experts that have “a minimum of 8 years of experience teaching neurologic content in physical therapy education programs” (Gorman & Lazaro, 2011, p. 64). After the validation, the OSCE will be field tested. It will help to better understand how students react to the proposed scenarios. After field testing, debriefing session will be conducted in order to elicit student responses that might help with adjusting the scenarios. The participants of field tests will be asked specific open-ended questions and will be offered standardized questionnaires with items related to the patient stations. After the end of the debriefing phase of the OSCE, all scenarios will be reviewed. The next phase of the OSCE development is the introduction of editorial changes based on the students’ feedback obtained in the previous phase. Appendix A shows the process of the development of a nursing assessment and evaluation plan.
References
Estes, M. (2013). Health assessment & physical examination (1st ed.). Albany, NY: Thomson Learning.
Gorman, S., & Lazaro, R. (2011). Development and implementation of an Objective Structured Clinical Examination (OSCE) in Neuromuscular Physical Therapy. Journal of Physical Therapy Education, 24(3), 62-71.
Levett-Jones, T., Gersbach, J., Arthur, C., & Roche, J. (2011). Implementing a clinical competency assessment model that promotes critical reflection and ensures nursing graduates’ readiness for professional practice. Nurse Education in Practice, 11(1), 64-69.
Mcwilliam, P., & Botwinski, C. (2012). Identifying strengths and weaknesses in the utilization of Objective Structured Clinical Examination (OSCE) in a nursing program. Nursing Education Perspectives, 33(1), 35-39.
Schub, E., & Heering, H. (2016). Clinical competencies: assessing. Journal of Professional Nursing, 45(7), 103-108.
Selim, A., Ramadan, F., El-Gueneidy, M., & Gaafer, M. (2012). Using Objective Structured Clinical Examination (OSCE) in undergraduate psychiatric nursing education: is it reliable and valid? Nurse Education Today, 32(3), 283-288.
Appendix A
Order from us for quality, customized work in due time of your choice.